Everything you should know about Gestational Diabetes
Key takeaways:
1 in 4 pregnancies in Singapore is affected by gestational diabetes.
Gestational diabetes is a condition in which high blood glucose (sugar) develops during pregnancy.
Uncontrolled gestational diabetes can lead to significant complications during pregnancy and delivery and increase the risk of diabetes in your child.
Effective management of gestational diabetes, includes a healthy diet, regular physical activity, regular monitoring of blood glucose, and may include medication.
Effective management can help to reduce the risk of complications during pregnancy and the birth of the baby by 58%.
What is gestational diabetes?
Gestational diabetes mellitus (GDM) or gestational diabetes is a condition where high blood glucose (sugar) develops during pregnancy. Having gestational diabetes doesn’t mean that you had diabetes before your pregnancy or will have it afterward. However, gestational diabetes does raise your risk of developing type 2 diabetes in the future. If poorly managed, it can also raise your child’s risk of developing obesity and diabetes, and increase the risk of complications for you and your baby during pregnancy and delivery.
Gestational diabetes can happen at any stage of pregnancy but is more common in the second or third trimesters. 1 in 4 pregnancies in Singapore is affected by gestational diabetes.
Why does gestational diabetes happen?
First, here is a quick introduction to how blood glucose (sugar) levels are regulated in the body.
After a meal, any carbohydrate that is consumed will be broken down into glucose, resulting in an increase in blood sugar levels.
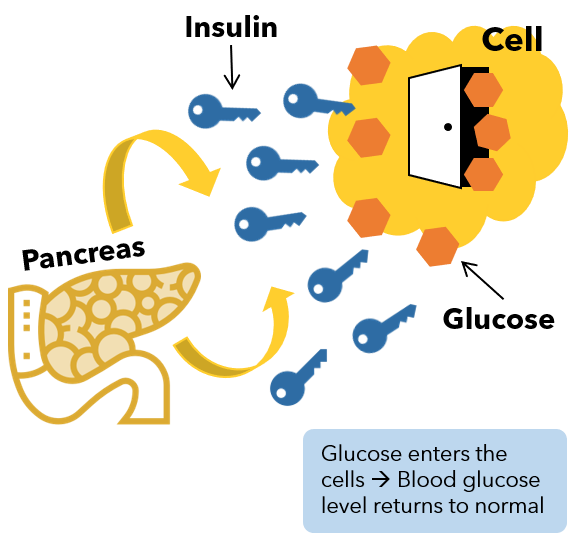
The pancreas detects this rise in blood glucose and will start to secrete insulin. Insulin acts like a key, allowing blood sugar to enter the cells in the body, where it can then be converted into energy (see Figure 1). Insulin thus helps to lower blood sugar levels.
Figure 1. Insulin acts as a “key” to help glucose enter our cells. When insulin doesn’t work effectively, glucose stays in our blood, leading to high blood sugar.
During pregnancy, your body and placenta produce higher amounts of some hormones, such as the human placental lactogen (hPL) and hormones that increase insulin resistance. Insulin starts to work less effectively on the cells, resulting in an increase in blood glucose levels. Most pregnant women can produce enough insulin to overcome this insulin resistance, but those who cannot develop gestational diabetes as the blood glucose levels rise abnormally.
Risk factors for gestational diabetes
Any woman can develop gestational diabetes during pregnancy, but some may be at an increased risk, for example, if they:
Have family members (i.e. parents or siblings) who have diabetes.
Are overweight or obese before pregnancy (BMI of ≥23 in Asians or ≥25 in non-Asians, especially if they have excess fat around the waist).
Are 40 years and older.
Had a child previously who weighed more than 4kg at birth.
Had a history of gestational diabetes during a previous pregnancy.
Are expecting multiple babies.
Gained a larger than normal amount of weight while you’re pregnant.
Have hypertension.
Signs and symptoms of diabetes
Typically, gestational diabetes is not associated with any symptoms. If you do experience symptoms, they tend to be mild and non-specific and can include increased thirst or increased frequency of urination. This is why it is important to go for screening in accordance with the guidelines to pick up gestational diabetes early.
Screening and diagnosis of gestational diabetes in Singapore
In Singapore, it is recommended that all pregnant women be screened for gestational diabetes at 24 to 28 weeks of gestation unless they have a history of pre-existing diabetes or pre-diabetes (1).
The Oral Glucose Tolerance Test (OGTT) is used to screen for gestational diabetes. You will first undergo a blood test in the morning to check your blood glucose level after 8-10 hours of overnight fasting. You will then be given a 75g glucose drink. Blood samples will be taken at the one- and two-hour intervals to assess how your body is dealing with the glucose.
Gestational diabetes glucose levels
Gestational diabetes is diagnosed if your fasting blood sugar level is 5.1mmol/L (92mg/dL) or greater, your 1-hour reading is 10mmol/L (180mg/dL) or greater, or your 2-hour reading is 8.5mmol/L (153mg/dL) or greater (1).
Screening for preexisting diabetes before pregnancy
If you have any of the following risk factors, you should be screened for preexisting diabetes before or during the first trimester of your pregnancy (1):
have a pre-pregnancy BMI of more than 30 kg/m2;
have a history of gestational diabetes;
have a history of polycystic ovary syndrome;
have a history of pre-diabetes;
have delivered a baby 4 kg and heavier;
are 40 years and older
To screen for preexisting diabetes, you will need to undergo a standard OGTT. This requires you to fast overnight and then drink a 75g sugary liquid at the doctor's office. Blood sugar levels are tested before the sugary drink and two hours after the drink. For the first reading, a reading of less than 5.6 mmol/L (100 mg/dL) is normal. A level from 5.6 to 6.9 mmol/L (100 to 125 mg/dL) indicates prediabetes. A reading of 7 mmol/L (126 mg/dL) or higher suggests you have diabetes. For the second reading (two hours after taking the sugary drink), a blood sugar level less than 7.8 mmol/L (140 mg/dL) is normal. A reading between 7.8 mmol/L and 11.0 mmol/L (140 and 199 mg/dL) indicates prediabetes. A reading of 11.1 mmol/L (200 mg/dL) or higher after two hours suggests diabetes.
If your test is normal, you should be screened for gestational diabetes at 24 to 28 weeks of gestation (1).
Complications and risks of gestational diabetes
While most pregnant women with gestational diabetes go on to deliver healthy babies, gestational diabetes can cause complications for mother and child if not properly managed, such as:
For the Mum:
Premature labor and premature birth
Increased likelihood of requiring induced labor
Risk of complicated delivery requiring a C-section
Pre-eclampsia – a condition that causes high blood pressure during pregnancy and can lead to pregnancy complications for both mum and baby if not treated
Higher risk of developing Type 2 diabetes and cardiovascular disease in the future (2,3,4)
For the Baby:
Macrosomia – excessive growth of the baby – which can increase risk of shoulder dystocia (where the baby’s shoulders become stuck after his head passes through the birth canal during labour)
Risk of developing low blood sugar (hypoglycaemia) shortly after birth, which may provoke seizures
Risk of becoming overweight or obese during childhood or adolescence
Increased risk of developing Type 2 diabetes (4,5)
Are there any long-term effects of gestational diabetes?
Your blood sugar usually returns to normal after delivery. A repeat OGTT is recommended at 6 to 12 weeks post-delivery to check if your blood sugar levels have returned to normal.
Women who have had gestational diabetes have a 20-70% risk of progressing to Type 2 diabetes in the first decade after delivery (1). You should, therefore, go for regular screening for diabetes or pre-diabetes at least once every three years. More frequent (yearly) follow-up may be required if you received insulin during pregnancy or if you have risk factors for developing diabetes, such as obesity or having a family history of diabetes.
Eating healthily and staying physically active can help you to delay or prevent the onset of Type 2 diabetes in the future (1).
If you have a history of gestational diabetes and are planning for another pregnancy, you should also get checked for diabetes before conception.
How to keep gestational diabetes under control?
If you have gestational diabetes, your treatment plan may vary depending on your blood sugar levels. In most cases, gestational diabetes is managed with :
Lifestyle interventions involving a healthy diet and adequate physical activity
Regular monitoring of blood glucose levels before and after meals and keeping your blood glucose levels within the target range
Oral medications or insulin injections may be necessary in 10 to 20 percent of women with gestational diabetes
Effective management of gestational diabetes can reduce the risk of complications during pregnancy and the birth of your baby, and reduce the risk of obesity and diabetes in your child.
If you have gestational diabetes, your doctor and health coach/dietitian will help to develop an appropriate care plan for you, but typical recommendations include the following:
What should I eat if I have gestational diabetes?
Eat a healthy diet with a good balance of vegetables, fruits, lean protein, and high-fibre carbohydrate foods.
Choose high fibre options when taking carbohydrates, for example brown rice, wholegrain bread, wholemeal pasta, oats, low sugar fruits. The fibre helps to slow the digestion and absorption of glucose into the bloodstream, resulting in lower and slower increases in blood sugar. Your dietitian and doctor will let you know how much carbohydrates you should consume each day.
Cut down your intake of sugary drinks, desserts and snacks. Overconsumption can result in excess calorie intake, leading to weight gain. Sugary items are also broken down quickly in the body, inducing rapid spikes in blood sugar levels.
Space out carbohydrate-rich foods. By breaking up your carbohydrates into smaller portions, for example eating half your sandwich at 8am and the other half at 10am instead of consuming the full sandwich at 8am, you will better control your blood sugar level.
Practice portion control. Avoid large portions of carbohydrates which will cause blood sugar levels to rise to unhealthy levels. As a general guide, carbohydrates like rice and noodles should only make up ¼ of your meals.
Should I exercise if I have gestational diabetes?
Pregnant women should ideally get at least 150 minutes of light to moderate-intensity physical activity (e.g. brisk walking) each week.
Some light activity such as walking is better than none and can help keep blood sugar levels in control, especially after food.
Your doctor can advise you on a safe level of activity for you and your baby throughout your pregnancy.
When does medication come in?
In 10 - 20% of mothers with gestational diabetes, dietary changes alone may not be sufficient to keep their blood sugar levels under control. In these situations, their doctors may suggest putting them on medication to keep the mother and baby safe during the pregnancy and delivery.
The two medications commonly used in these instances are metformin and insulin. Both medications are safe for use in pregnancy. If you are on medication for gestational diabetes, be sure to monitor your blood sugar level regularly. This helps you and your doctor monitor response to therapy, and make any necessary adjustments in a timely manner.
How often should I measure my blood sugar level?
It is important to monitor your blood sugar level if you have gestational diabetes so that you know if you are keeping your gestational diabetes under control, and how you are responding to treatment.
You may monitor your condition using a glucometer and test strips, or using a continuous glucose monitor.
Ideally, you would need to measure your blood sugar level when you wake up, before each meal and 1 to 2 hours after food.
How frequently you need to monitor your blood sugar level may vary depending on your condition and should be discussed with your doctor.
What is the normal blood sugar range if I have gestational diabetes?
If you have gestational diabetes, you should aim to keep your blood sugar level within the following ranges (1):
Before food: < 5.3 mmol/L (<95mg/dL)
1-hour after food: < 7.8mmol/L (<140mg/dL)
2-hour after food: <6.7mmol/L (<120mg/dL)
Can I breastfeed if I have gestational diabetes?
Breastfeeding is recommended for all women, including women with gestational diabetes. Breastfeeding provides many benefits to your baby (including reducing the risk of obesity and diabetes in your baby), and also helps you to return to your pre-pregnancy weight (6).

Getting support
We understand that gestational diabetes can cause undue stress and anxiety to mothers. With the huge amount of information online about gestational diabetes, it can be difficult to sieve out the key information you need to be confident in managing your blood sugar.
We hope that this resource hub is useful to you. If you need someone to help you out, our doctors and health coaches are always here for you! We will work with you to figure out an ideal plan for you. Not only that, we will also be with you every step of the way to provide support whenever and wherever you need it.
References
Agency for Care Effectiveness (ACE), 2008. Gestational diabetes mellitus: An update on screening, diagnosis, and follow-up. http://www.ace-hta.gov.sg/public-data/our-guidance/GDM%20-%20An%20update%20on%20screening,%20diagnosis%20and%20follow-up%20(May%202018).pdf
Bellamy L, et al. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet. 2009.
Carr D. B., et al. Gestational Diabetes Mellitus Increases the Risk of Cardiovascular Disease in Women With a Family History of Type 2 Diabetes. Diabetes Care 2006 Sep; 29(9): 2078-2083.
Hartling L, et al. Benefits and harms of treating gestational diabetes mellitus: a systematic review and meta-analysis for the U.S. Preventive Services Task Force and the National Institutes of Health Office of Medical Applications of Research. Ann Intern Med. 2013.
HAPO Study Cooperative Research Group. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008.
Gunderson, E. P. Breastfeeding After Gestational Diabetes Pregnancy : Subsequent obesity and type 2 diabetes in women and their offspring. Diabetes Care 2007 Jul; 30(Supplement 2): S161-S168.