Does Diabetes Cause Mood Swings and Fatigue (And Tips To Feel Better)
Takeaways
Blood sugar fluctuations can negatively impact your mood and energy levels.
Large blood sugar spikes and dips often stem from consuming considerable amounts of simple carbohydrates in a single sitting. This results in an especially dramatic “crash and burn” effect (i.e., reactive hypoglycemia) in individuals with diabetes since their insulin responses don’t work properly.
Reactive hypoglycemia may cause symptoms like irritability, anxiety, fatigue, and difficulty concentrating.
A continuous glucose monitor (CGM) helps you discern if you're experiencing blood sugar fluctuations. This, in turn, allows you to take the necessary steps to "flatten" your glucose curve—and take control of your mood and energy levels.
You can prevent large blood sugar fluctuations by eating healthy foods, staying physically active, and managing stress levels.
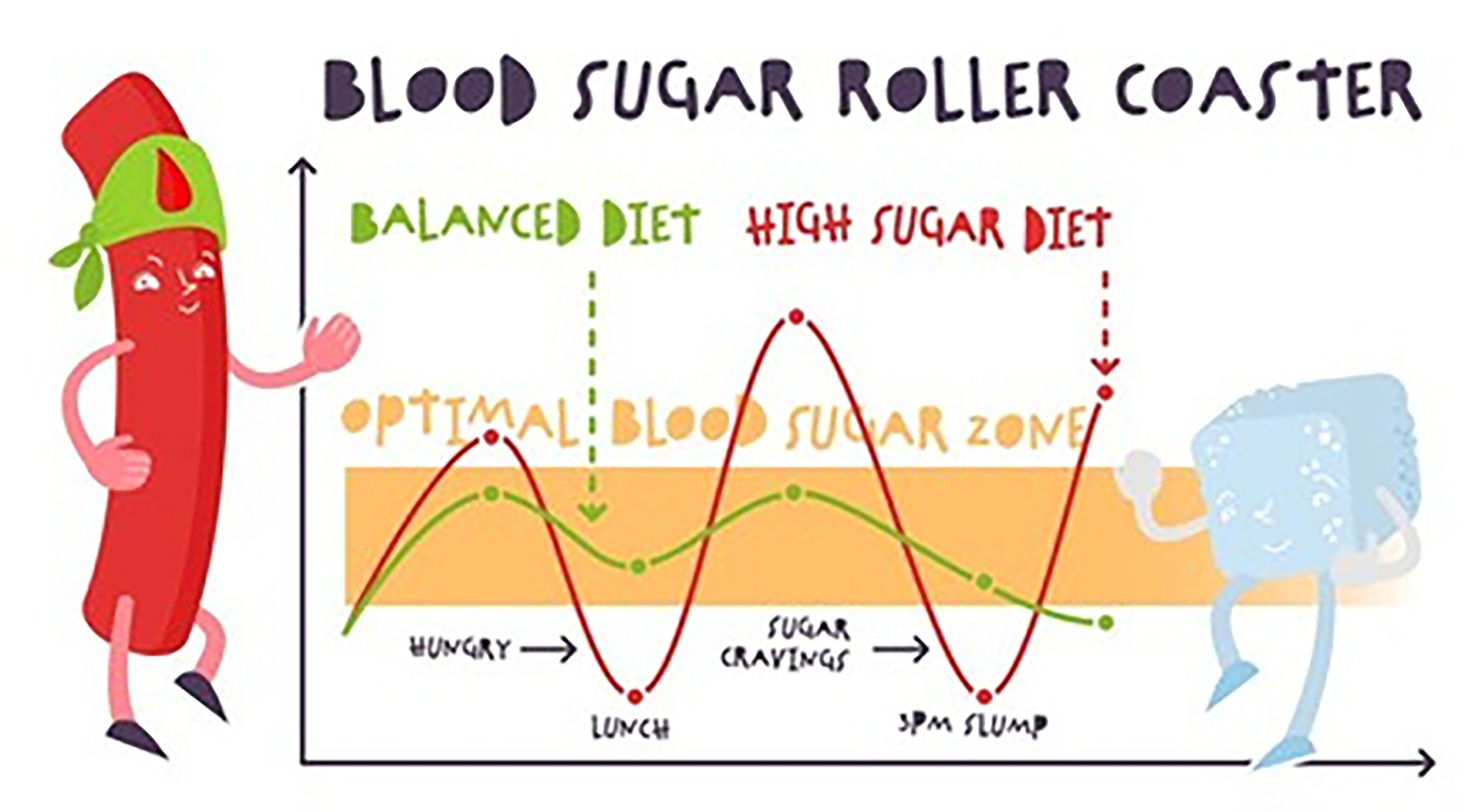
Blood sugar fluctuations or "glycemic variability"—a characteristic of poorly controlled glucose levels—could negatively impact your mood. More specifically, hypoglycemia (i.e., low blood sugar) has been associated with "nervousness", and hyperglycemia (i.e., high blood sugar) with "anger or sadness". Imaginably, the constant cycling between the highs and the lows can make you feel like you’re on an emotional rollercoaster, which seems impossible to get off.
The adverse impact of blood sugar fluctuations on your mental well-being extends beyond a mishmash of complicated emotions. It is also associated with chronic fatigue, linked to a higher risk of depression. This, in turn, explains why individuals with diabetes are 2 to 3 times more likely to experience depression. Thankfully, you can take steps to avoid large blood sugar spikes and dips.
This article explores the relationship between blood sugar fluctuations, mood, and energy levels—plus gives you tips on how to flatten your blood glucose curve so you function at and feel your best.
How blood sugar fluctuations cause mood swings and fatigue
To understand how blood sugar fluctuations cause mood swings and fatigue, you’ll first need to know the basics of carbohydrate metabolism. So, let’s start there.
When you consume carbohydrates (e.g., pasta and biscuits), your body breaks them down into glucose molecules—which eventually enter the bloodstream. The rising blood glucose levels then signal the pancreas to secrete insulin, a hormone responsible for absorbing the excess glucose in the blood.
Under normal circumstances, the synchronized “dance” between blood glucose and insulin levels keeps sugar levels nice and steady.
As you’ve probably suspected, though, there are instances where this fails to occur. Why? The number one culprit: consumption of a large concentration of simple carbohydrates (e.g., fried horfun for lunch) in a single sitting.
Here’s how that plays out in people with and without diabetes:
Individuals without diabetes: Simple sugars are digested and absorbed into the bloodstream really quickly (compared to complex carbohydrates). This often leads to a rapid and dramatic spike in blood sugar levels, resulting in an initial jolt of energy and a corresponding uplift in your mood soon after eating. However, this doesn’t last. As mentioned earlier, the body will secrete insulin to counter the rise in blood sugar levels. As insulin levels “catch up” in response and peak, blood glucose levels will fall quickly. Essentially, this creates a “crash and burn” effect (i.e., reactive hypoglycemia) associated with symptoms like fatigue and irritability.
Individuals with diabetes: In people with diabetes, blood sugar fluctuations’ negative impact on mood and energy levels can be even more pronounced. That’s because insulin responses don’t work properly. Glucose levels may thus rise higher and for longer than those without diabetes (i.e., a higher and more sustained peak)—which also brings about a steeper corresponding decline in sugar levels once corrected with diabetes medication, like insulin therapy.
Note that beyond fatigue and irritability, reactive hypoglycemia may also cause:
Weakness
Anxiety
Dizziness
Palpitations
Difficulty concentrating
Blurred vision
Sweating
Tremor or shakiness
How to determine if you are experiencing blood sugar fluctuations
As mentioned earlier, symptoms of reactive hypoglycemia include fatigue, weakness, anxiety, irritability, and If you notice any of these symptoms, you may be experiencing blood sugar fluctuations. That said, it’s also worth noting that these symptoms may not necessarily result from glycemic variation.
So, this begs the question: how can you tell for sure if you’re indeed experiencing blood sugar fluctuations? Well, that’s where continuous glucose monitoring devices come into play.
With a continuous glucose monitor, you are able to easily and painless track your glucose levels, and see if there are any rapid fluctutations, or low or high glucose events that correlate with mood and energy changes. This device uses an electrode under the skin to read your blood sugar levels at regular intervals, usually 5 to 15 minutes. This information is then transmitted to a separate device for you to read, or to an insulin pump.
Continuous glucose monitoring helps you flatten your glucose curve by showing you blood sugar trends throughout the day. You can use this information to identify the causes of your blood sugar spikes, which is priceless to gain more control over your blood sugar levels. Since you receive information in real-time, you can also prevent sugar spikes or get timely help when you notice a spike. This, in turn, allows you to “optimize” your mood and energy levels.
What does flattening the glucose curve look and feel like?
Here’s a disclaimer, though: “flattening” your glucose curve doesn’t entail keeping your blood sugar levels at a constant (i.e., flat line). Instead, all it means is a reduction of massive spikes and dips, where you maximize your time spend in the optimal blood sugar zone—so you feel more energetic, alert, productive, and in-control of your emotions.
3 simple tips to prevent blood sugar spikes
You can control your spikes through diet, exercise, and lifestyle changes.
Tip #1: Eat healthy foods to keep your blood sugar in check
Carbohydrates, especially those that are refined, are the main culprit of blood sugar spikes. Some typical high-carb foods include:
Sugary foods and beverages drinks like cakes, soft drinks and fruit juices
Refined grains like white bread, rice and noodles
Starchy vegetables like potatoes, sweet potatoes
You can replace those foods with better alternatives that are less likely to spike your blood sugar. Some examples include:
Whole grains which are minimally processed and therefore contain more fiber such as brown rice, buckwheat, quinoa and bulgur
Non-starchy vegetables such as leafy greens, capsicums and tomatoes.
Legumes and beans such as chickpeas, lentils and soybeans.
Fresh fruits such as berries, kiwifruit and apples
Plain dairy products without added sugar
Whichever you choose, keep in mind that the portion that you eat also matters. Also, it's a good idea to drink plenty of water throughout the day to keep yourself hydrated - that way, you'll be less likely to experience sugar spikes.
Tip #2: Stay active to help your body manage sugar levels
When you are active, your body’s insulin sensitivity increases. In other words, the insulin that your pancreas produces will be more effective. Exercising also helps you control your blood sugar levels. In addition, regular activity is a great way to manage your body weight. People with high body weight have a much harder time keeping their blood sugar under control. One study showed that people who lost 14 pounds saw their blood sugar drop by 14%.
Another study shows that if you lose 10% or more of your body weight, you're twice as likely to achieve remission for type 2 diabetes. In one study, participants achieved this without any intensive lifestyle interventions or extreme calorie restrictions - so it's definitely doable!
For the best results, aim for at least 20 to 25 minutes of activity every day. However, be sure to check your blood sugar levels before exercising as too low (below 4 mmol/L) or too high (above 13mmol/L) sugar levels can be dangerous.
Tip #3: Tweak your lifestyle to improve your mood and sugar levels
When you feel stressed, this affects your mood and your blood sugar at the same time. Your body's natural response to stress releases sugar into your bloodstream for energy. This can lead to blood sugar spikes, especially if you're not getting enough sleep.
Luckily, you can manage your mood and blood sugar levels through meditation, healthy sleep habits, and relaxing nature walks.
Another positive lifestyle change for blood sugar control is surrounding yourself with a support group. This can give you an outlet to express any fears, stress or challenges you're facing. With like-minded people by your side, you'll be better equipped to manage your blood sugar levels effectively.
Manage Your Blood Sugar Levels with Expert-Level Help
Here at NOVI, we're dedicated to providing you with the best possible care for your diabetes.
Our team of experts will work with you to develop a holistic strategy that fits your needs and makes you feel comfortable. We care about our clients and their feelings, so you can be sure that you're in good hands.
Feel free to talk to our expert coaches about your specific situation, and we’ll create a personalized, easy-to-follow action plan to help you reduce blood sugar spikes, avoid mood swings, and enjoy life to the fullest. Don't allow diabetes to control your life!