How to Interpret Your Cholesterol Numbers
Key Takeaways
Cholesterol is a fatty substance which is important for many functions in the body, including making cell membranes as well as many hormones.
Cholesterol is carried in the blood on proteins known as lipoproteins.
Increased levels of low-density lipoprotein, or LDL, are associated with an increased risk of heart attacks and strokes.
Increased levels of high-density lipoprotein, or HDL, are associated with a decreased risk of heart attacks and strokes.
Increased levels of triglycerides, another type of fat in the blood, are also associated with an increased risk of heart attacks and strokes.
A standard cholesterol test, also known as a lipid panel, measures your total cholesterol along with HDL, LDL, and triglycerides. This is recommended at least once every three years starting at age 40, and sooner and/or more often for some people.
There are also other blood tests that can be used to determine a person’s risk of heart disease, which may be used in certain cases.
Cholesterol is a fatty substance which is produced by the liver and is also absorbed from foods. Cholesterol is actually important for health. It’s a component of cell membranes, which surround every cell in the body. In addition, it’s used as a building block for many different substances in the body, including certain hormones, vitamin D, and bile acids (which are used to digest fat). Without cholesterol, the body would not be able to function well.
At the same time, high cholesterol levels have been associated with an increased risk for health issues, like heart attack and stroke. It’s recommended to get your cholesterol levels tested. As part of a cholesterol test, the levels of certain other types of fats in the blood are also tested. This gives a complete picture of a person’s risk for heart disease, so they can take action as needed to help reduce their risk.
Who should get their cholesterol tested?
In general, the Ministry of Health recommends that everyone have their cholesterol tested regularly, starting at age 40. If the results are within the normal range, then the test should be repeated once every three years.
Certain people may need to start screening at an earlier age and/or to have their cholesterol tested more frequently. These include people who:
Have family members who had heart attacks or strokes at a relatively early age (younger than age 65)
Have multiple family members with high cholesterol
Have previously experienced a heart attack or stroke
Have a condition that increases the risk of heart disease, such as diabetes or obesity
Are current smokers, or have quit smoking recently
Have had abnormal results on a previous cholesterol test
If you believe that it’s time to get your cholesterol tested, make an appointment with your doctor. They can advise you on whether a cholesterol test is recommended for you, and can order it from a lab if so. They will also advise you about any other screening tests that may be recommended, based on your age, family history, and health status.
What do your cholesterol numbers mean?
A cholesterol test does not simply measure your overall cholesterol level. Your test results will contain multiple different measurements related to your cholesterol, and each one means something different for your health. Two of the main measurements reported are your levels of HDL and LDL.
What are HDL and LDL?
Because cholesterol is a fatty substance, it cannot dissolve directly in blood, which is made up of water. Instead, the body makes protein scaffolds to carry cholesterol through the bloodstream. These are known as lipoproteins.
There are multiple different types of lipoproteins, and they have different functions. High-density lipoproteins, or HDL, act to gather cholesterol from tissues throughout the body and bring it back to the liver, where it can be reused or eliminated. Low-density lipoproteins, or LDL, bring cholesterol to the tissues of the body, so that it can be used.
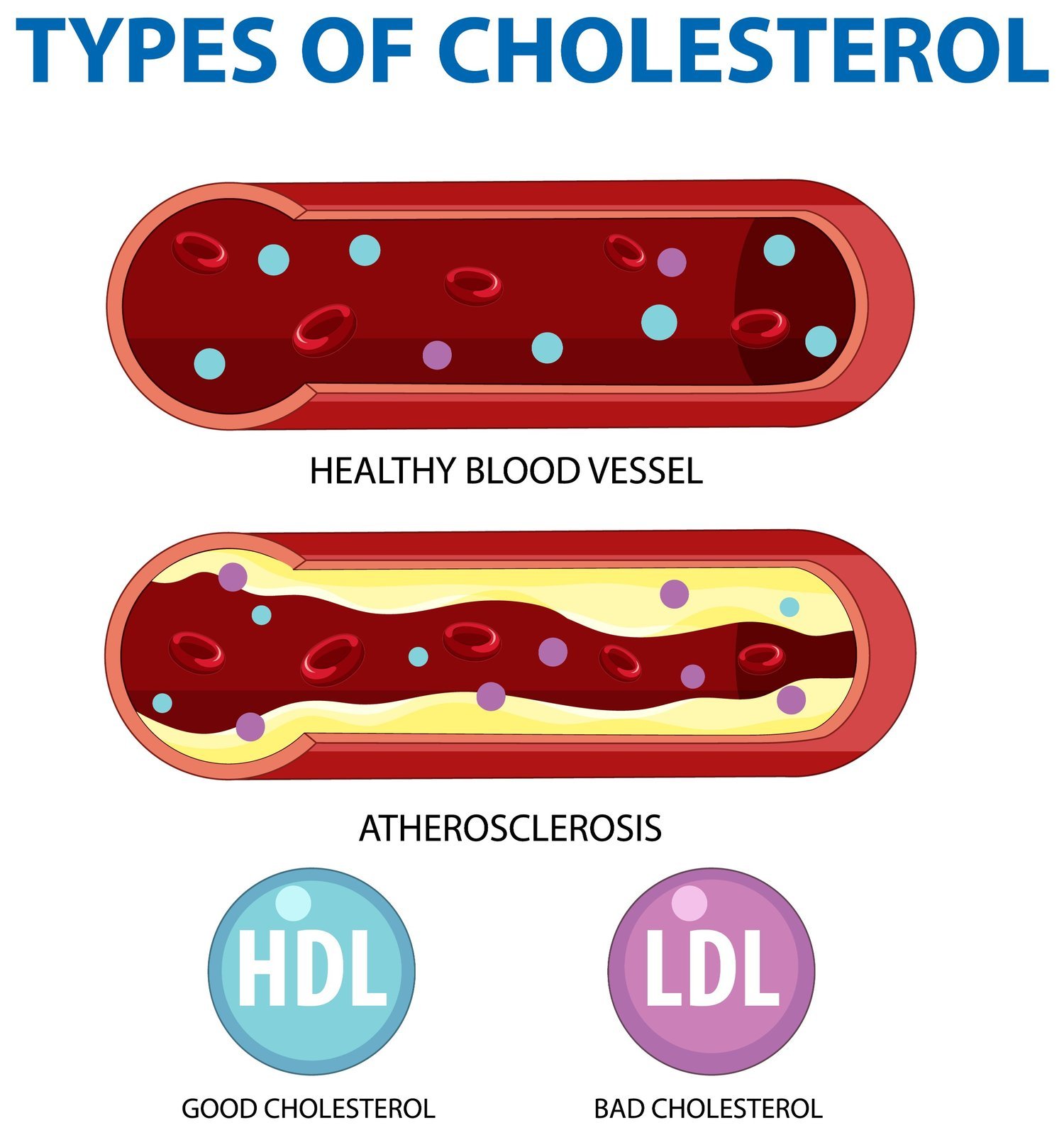
Research has found that higher levels of HDL are associated with a lower risk of heart attacks and strokes. This is why HDL is sometimes known as “good cholesterol.” By scavenging excess cholesterol and returning it to the liver, HDL helps to prevent cholesterol from building up in blood vessels.
By contrast, higher levels of LDL are associated with a higher risk of heart attacks and strokes. This is why LDL is sometimes known as “bad cholesterol.” When there’s too much cholesterol in the body, it can start to deposit in the walls of blood vessels. This narrows the blood vessels, which makes them stiffer and reduces blood flow. It also increases the risk that a blood clot will form, which can block a blood vessel completely. LDL keeps cholesterol in the bloodstream rather than returning it to the liver, which increases the chances that it will deposit in the walls of blood vessels.
What are triglycerides?
As part of a lipid panel, your triglyceride levels are tested along with your total cholesterol, HDL, and LDL levels. Triglycerides are not a type of cholesterol, but they are a type of fat. Triglycerides are the fats that your body uses to store excess energy. These circulate in your blood and are available to cells to use as energy or to store for later. Triglycerides are carried on very low density lipoprotein, or VLDL.
Triglycerides can also deposit into the walls of blood vessels. Because of this, high levels of triglycerides are also associated with an increased risk for heart disease.
What is a normal or healthy cholesterol reading?
Based on the results of a lipid panel, doctors can determine a person’s cardiovascular risk, which is the risk of having a heart attack or stroke over the next ten years. For total cholesterol, LDL, and triglycerides, lower levels indicate lower risk, while higher levels indicate higher risk. For HDL, it’s the opposite, with higher levels indicating lower risk.
| Total Cholesterol (mmol/L) | LDL (mmol/L) | HDL (mmol/L) | Triglycerides (mmol/L) | |
|---|---|---|---|---|
| Desirable | Less than 5.2 | Less than 3.4 | 1.0 to 1.5 | Less than 2.3 |
| Borderline High | 5.2 to 6.1 | 5.2 to 6.1 | ||
| High | 6.2 or higher | 4.1 or higher | 1.6 or higher | 2.3 or higher |
Source: Health Promotion Board of SingaporeStudies have shown that, for every increase in LDL of 40 mg/dL over the baseline of 100 mg/dL, the risk of having a heart attack or stroke increases by 34%. For those in older age groups, the increase in risk is even higher.
Although cholesterol levels are one factor that indicates your risk, there are also many other factors that influence your cardiovascular risk, including:
Age
Smoking
Alcohol consumption
Family history
Diet
Physical activity levels
Medical conditions
It’s important to take these factors into account when interpreting the results of a cholesterol test. Your doctor will help you to interpret your test results, in the context of your personal situation.
The HDL Ratio
HDL is protective against heart disease. The greater the percentage of your total cholesterol that’s made up of HDL, the more protected you are against heart disease. To assess this percentage, the HDL ratio is used.
To calculate your HDL ratio, divide your total cholesterol by your HDL. For example, if your total cholesterol is 240 mg/dL and your HDL is 40 mg/dL, your HDL ratio would be 6:1 (or 6 to 1). As your HDL increases, your HDL ratio will decrease. With the same total cholesterol of 240 mg/dL, if your HDL is 60 mg/dL, then your HDL ratio would be 4:1.
A normal HDL ratio is 5:1 or less. An HDL ratio above 5:1 means that your HDL is low relative to your total cholesterol, which is an indicator of risk. The HDL ratio is considered very healthy if it’s 3.5:1 or less.
Other lipoprotein tests
While a standard lipid panel contains tests of total cholesterol, HDL, LDL, and triglycerides, there are some newer blood tests that doctors have been finding are also useful for assessing a person’s cardiovascular disease risk. These are not necessarily recommended as screening tests for everyone. However, they may be used in certain cases, to help get a better picture of your cardiovascular disease risk.
Lipoprotein (a)
Lipoprotein (a) is a specific type of LDL. Levels below 14 mg/dL are considered optimal. Up to 30 mg/dL is borderline high, while levels above this indicate high risk.
Unlike with other types of cholesterol, your levels of lipoprotein (a) are almost entirely determined by genetics. This test is sometimes recommended for people who have a strong family history of heart disease. Even if your LDL levels are low and your HDL levels are high, high lipoprotein (a) could mean that you’re at an increased risk for a heart attack.
There isn’t a lot that you can do to alter your lipoprotein (a) levels. However, if your levels are high, then it’s even more important to take other steps to reduce your cardiovascular risk.
Apolipoprotein A1 and apolipoprotein B
Apolipoprotein B-100, generally known as apolipoprotein B or apo B, is a structural component of both LDL and VLDL. Measuring apo B levels can therefore provide a measurement of both of these harmful components at the same time. Apolipoprotein A1, or apo A1, is a structural component of HDL cholesterol. Higher apo B levels indicate an increased cardiovascular risk, while higher apo A1 levels indicate decreased risk. In general, apo B levels should be less than 130 mg/dL, while apo A1 levels should be at least 75 to 80 mg/dL.
Research has shown that the ratio between apo B and apo A1 may be more predictive of a person’s risk of heart disease than other blood tests are. When the apo B/A1 ratio is less than 0.7, this indicates average risk. A ratio of 0.9 or higher indicates high risk.
Testing of apo A1 and B levels is not part of a standard lipid panel, but may be performed in cases where it would be helpful to have an additional way to assess a person’s risk. For example, people with a strong family history of heart disease or those who have personally experienced a heart attack already may benefit from this testing.
Lowering your cholesterol levels
If you have high levels of LDL cholesterol, then taking steps to reduce these may help to reduce your risk of heart disease. There are a few different ways to do this. Some of these involve lifestyle changes, while others involve prescription medications. Talk with your doctor about the best options for you, and make a plan together for addressing your high cholesterol levels.
Diet
The foods that you choose to eat can make a difference in your cholesterol levels. The following nutritional guidelines can help to lower LDL:
Eat less saturated fat (found in red meat, butter, full-fat dairy, and coconut oil)
Eat less trans fat (found in packaged foods)
Eat more monounsaturated and polyunsaturated fat (found in most vegetable oils as well as avocados, nuts, and seeds)
Eat more fiber (found in whole grains, fruits, and vegetables)
The amount of cholesterol that you take in through your diet can also make a difference. Cholesterol is found in egg yolks, meat, butter, and full-fat dairy. However, the impact of dietary cholesterol has been found to be relatively modest, which is believed to be because the body adjusts its own production of cholesterol to account for whatever is taken in through diet. While this may make an impact, other dietary factors are likely to be more important.
Plant Sterols
Plant sterols, also known as phytosterols, are compounds found naturally in many plant foods. Studies have found that consuming plant sterols can lower LDL cholesterol by about 8 to 12%. It’s thought that this occurs because plant sterols have a structure similar to that of cholesterol, so they compete with cholesterol for absorption in the digestive system. When you eat plant sterols, your body absorbs less cholesterol from your diet, which lowers your overall cholesterol levels.
Foods that contain higher levels of plant sterols include:
Legumes
Vegetables
Fruits
Seeds
Nuts
Whole grain products
Vegetable oils
Some food products are enriched with extra plant sterols. In addition, it’s possible to take plant sterols as a supplement. In general, getting your plant sterols through eating whole foods is likely to be the most beneficial. If you’re considering taking a supplement, make sure to talk to your doctor first to ensure that the supplement you’re considering will be safe for you.
Medications
There are also prescription medications that are used to lower LDL cholesterol levels. These medications are not a replacement for lifestyle factors like exercise and a healthy diet. However, in some cases, they can be a useful addition to a healthy lifestyle, helping to bring cholesterol levels down into a more normal range.
The most common type of cholesterol-lowering medication are statins. These medications are usually tried first. If lifestyle factors and statins aren’t enough to bring LDL levels into a healthy range, then other medications can also be added. Options include medications that decrease cholesterol absorption in the digestive tract, and PCSK9 inhibitors, a group of injectable medications that act by increasing receptors in the liver that help it to clear cholesterol from the bloodstream.
While cholesterol-lowering medications have been found to be effective at preventing heart attacks and deaths, they do carry side effects. It’s important to carefully consider the potential risks and benefits, and to be monitored while taking these drugs. If your doctor recommends cholesterol-lowering drugs, they’ll discuss the potential risks with you and let you know what to watch out for.
Weight Loss
In people who are significantly overweight, weight loss can help to reduce LDL levels and also raise HDL levels. Losing even 5% of body weight can make a significant difference in a person’s LDL levels and their cardiovascular risk. Some people are able to achieve this through diet and exercise alone, while others use medical weight loss to help them lose weight.