How does exercise help with blood sugar control?
Key Takeaways:
Exercise, along with diet, helps keep your blood glucose in check
Regular exercise enhances the effectiveness of insulin, the hormone responsible for regulating blood sugar
Aim for a combination of aerobic and strength/resistance training for optimal results.
While your diet plays a central role in managing blood sugar levels, exercise is equally important in keeping your blood glucose in check — whether you’re looking to prevent blood sugar spikes or reverse pre-diabetes. Here's how it works and some practical advice to help you get started.
The Link Between Exercise and Blood Sugar Control
In a nutshell, exercise could help you keep your blood sugar levels under control by promoting muscle growth and fat loss. It also improves general health and wellbeing.
After a meal, blood glucose levels rise as food is broken down and absorbed in the gut. This triggers an increase in insulin, the hormone responsible for transporting glucose to the muscles for energy use or storage. However, in individuals with metabolic conditions such as diabetes, this process is impaired. This causes blood sugar levels to rise to higher-than-ideal levels after eating.
Rapid spikes and drops in glucose levels often lead to an energy crash or “slump.” Over time, these blood sugar fluctuations can reduce the body's ability to use insulin effectively, a condition known as reduced insulin sensitivity or insulin resistance.
Studies show that exercise stimulates several processes within the body that lead to favorable changes in glucose metabolism and insulin sensitivity. Exercise was found to dramatically boost glucose uptake throughout the body by as much as 50 times when compared to rest.
Here are some ways how exercise can help with blood sugar regulation:
When you exercise, your muscles use glucose from your bloodstream, lowering blood sugar levels. Even a simple 10-minute walk after meals can significantly reduce post-meal blood sugar spikes.
Resistance training builds muscle mass, and since muscles burn more energy at rest than fat, having more muscle contributes to better glucose control.
Exercise boosts insulin sensitivity for up to 72 hours, meaning your body can store glucose more efficiently, preventing large spikes in blood sugar levels.
Exercise helps reduce body fat. In people with obesity, fat cells can cause low-level inflammation, impairing insulin’s function. Losing fat improves insulin sensitivity.
Exercise enhances sleep quality. Poor sleep can lower insulin sensitivity, so by improving sleep, exercise also aids in blood sugar regulation.
Exercise lowers stress by reducing cortisol, a hormone that counteracts insulin and raises blood sugar levels. This helps maintain better blood sugar control.
Exercise also has numerous benefits for individuals with diabetes, including:
Regular aerobic exercise, such as walking, running, or swimming, has been shown to significantly reduce Hemoglobin A1c (HbA1c) levels. In patients with type 2 diabetes, consistent aerobic exercise can reduce HbA1c by 0.5 to 0.7%. Even a modest reduction in HbA1c can lower the risk of complications like heart disease, kidney issues, and neuropathy.
Regular exercise benefits the body and brain, which contributes to longer healthspan. Physically, it strengthens muscles, improves cardiovascular health, and helps maintain a healthy weight, all of which reduce the risk of diseases like heart disease, stroke, and type 2 diabetes. Cognitively, exercise enhances brain function by promoting neurogenesis, improving memory, and protecting against neurodegenerative diseases like Alzheimer's and dementia.
Exercise plays an important role in weight management by increasing calorie expenditure and improving metabolism. When paired with a balanced diet, exercise can help you lose weight, particularly body fat, which often leads to improved physical appearance. Strength training and aerobic exercise can improve muscle tone, posture, and overall body composition, resulting in a leaner, more fit physique.
Strengthening muscles around problem areas such as the knees and back can provide much-needed support and alleviate pain. Engaging in targeted exercises can improve mobility, reduce the risk of injury, and enhance the quality of daily life.
Consistent exercise is essential for managing insulin resistance, as it enhances glucose metabolism and supports cardiovascular health. Both aerobic activities and strength training play a role in improving insulin sensitivity.
Building muscle mass increases your basal metabolic rate (BMR), which means your body burns more calories even at rest. As a result, people with more muscle mass often find it easier to maintain or lose weight while enjoying a more flexible diet. Strength training helps prevent muscle loss that occurs naturally with aging, and the increased muscle mass allows you to enjoy occasional indulgences without as much worry about weight gain. Additionally, muscle mass improves glucose metabolism, making it easier for your body to handle carbohydrates and reducing the risk of insulin resistance.
How Walking After a Meal Improves Your Blood Sugar Levels
Continuous Glucose Monitors (CGMs) provide real-time data on your blood sugar levels. A CGM uses a sensor that is inserted under the skin to measure your sugar level every few minutes.
A common observation among CGM users is the significant improvement in blood sugar control when they engage in light activity, like walking, after eating.
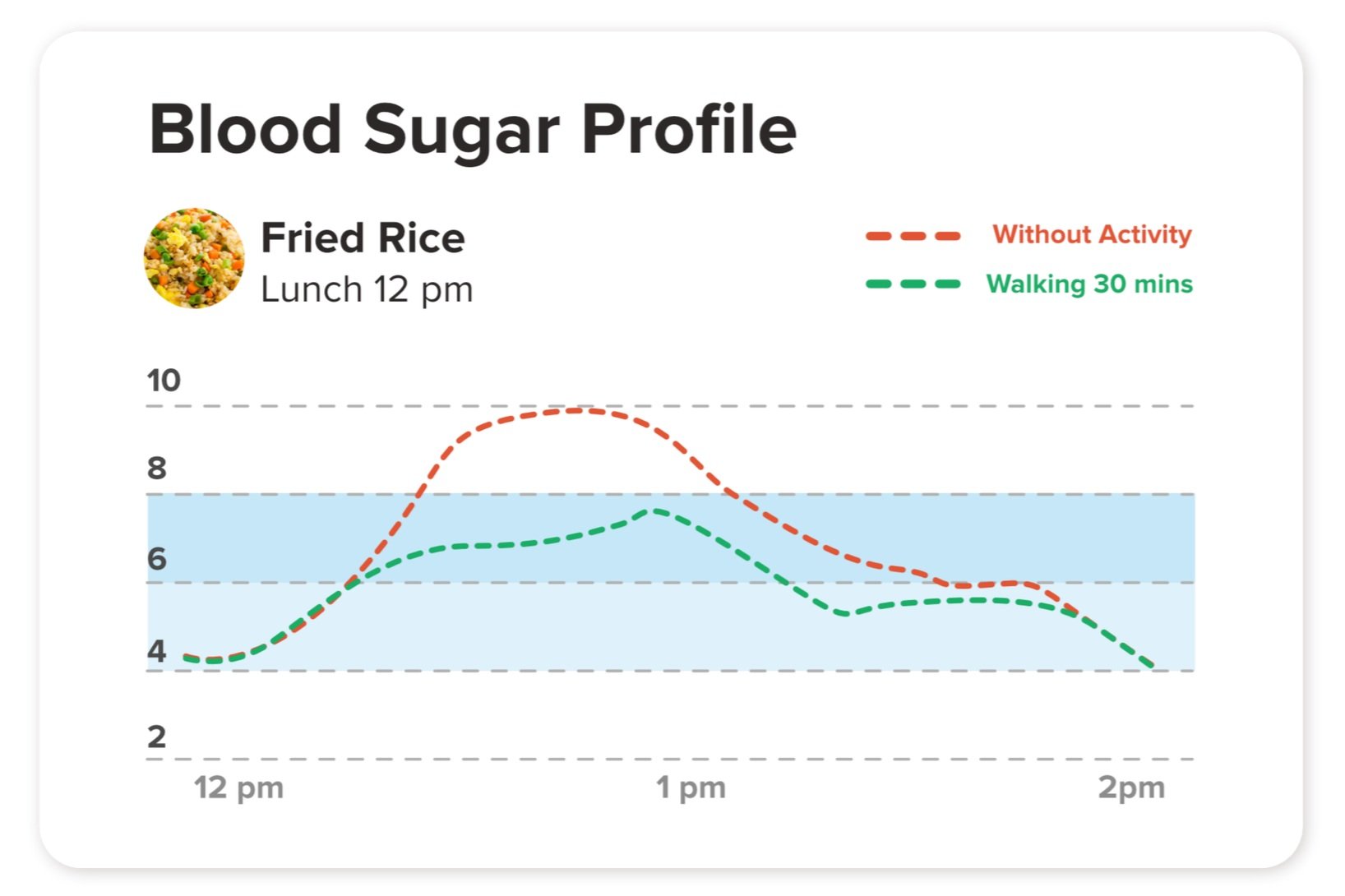
For example, a person who walks for 30 minutes after lunch might see a notable decrease in their post-meal blood glucose spike. Without walking, blood sugar might rise sharply, but a simple post-meal stroll can flatten the spike, helping to keep levels stable. Over time, this reduction in postprandial blood sugar spikes can have a substantial impact on overall glucose control.
Post meal glucose comparison between no activity and walking for 30 minutes
A study which analyzed 51 reviews on the effects of aerobic exercise on glucose and insulin levels after meals revealed that a single session of cardiovascular exercise – such as walking – within 6 hours of a meal caused a substantial reduction in blood glucose levels, compared to not exercising at all after a meal. Another study found that a combination of aerobic and resistance training significantly improved the hemoglobin A1c (HbA1c) of participants.
The Role of Muscles in Blood Sugar Control
Your muscles are the major metabolic sink for glucose disposal after a meal. Both exercise and insulin act synergistically to improve glucose disposal in your muscle. The greater your muscle mass, the more glucose your body can store and burn.
This is why resistance training and strength-building exercises are especially useful for blood sugar management. Resistance and strength training exercises increase muscle mass, which essentially expands your body’s capacity to handle glucose more efficiently.
How to Get Started
The idea of exercising to manage blood sugar might feel overwhelming. But you don’t need to spend hours at the gym to see results. When it comes to habit change, evidence tells us that having a plan and strategy is equally important as understanding why the change is beneficial. Here are 5 tips to turn exercising into a regular habit:
Ease into it. If you’re not used to exercising, begin with simple activities like a 10-minute walk after meals. This can make an immediate difference in post-meal blood sugar spikes.
Gradually increase your exercise intensity. As you build stamina, increase the length and intensity of your workouts. You could aim for a brisk 30-minute walk, light jogging, or swimming. Aim for at least 30 minutes of aerobic exercises most days of the week. For busy individuals, you can break up the exercise into shorter periods of about 10 minutes each time, aiming for a minimum of 30 minutes at the end of the day.
Incorporate strength training. Building muscle is essential for blood sugar control. Start with bodyweight exercises like squats, push-ups, or light weights. Even two or three strength-training sessions per week can make a noticeable difference. Strength training helps increase lean muscle mass which will raise your metabolism and burn more calories. These resistance-type exercises support strong, healthy bones. Building more muscle in place of fat is particularly important for those with type 2 diabetes because muscles use glucose, so the more you use your muscles, the more effective you can be at controlling your blood glucose level.
Consistency is key. It's better to exercise regularly in small amounts than to have occasional, intense sessions. Aim for at least 150 minutes of moderate-intensity aerobic activity per week, spread out over several days.
Listen to your body. If you have any health conditions or concerns, consult your doctor before starting a new exercise regimen. It’s also important to stay hydrated and avoid exercising on an empty stomach to prevent blood sugar dips.
If you have already signed up for our holistic NOVI Magnum diabetes treatment program and would like to maintain your blood sugar levels through a health coach-guided exercise, NOVI Optimum Fit is for you.
With NOVI Optimum Fit, you get:
1:1 personal training sessions with experienced coaches who will guide you through the workouts to ensure that they are safely executed.
Fitness coaches who are experienced at creating personalized training programs for individuals with medical issues.
Training programs that are flexible and constantly evolve with your progress.
Regular measurements of body fat percentage and muscle mass so you can track the results of your efforts.
Fitness coaches who work closely with NOVI doctors or dietitians to ensure that the training program complements your nutrition plans and medications taken.
A personal fitness coach who will keep you motivated and accountable for your fitness.