Everything you should know about Diabetes in Singapore
Key takeaways:
Diabetes is a condition where your blood glucose is abnormally high.
Poorly controlled diabetes increases your risk of serious complications such as heart disease, stroke and kidney failure.
You can keep your blood glucose under control by managing your lifestyle (healthy diet and regular exercise) as well as taking your prescribed medications.
This will help to reduce your risk of developing diabetes-related complications.
Improving your lifestyle may not be as difficult as you think if you know what exactly to aim for and the correct strategies to use!
You should monitor your condition regularly, and check for early signs of diabetes-related complications.
This article is written by NOVI Health’s specialist doctors (Dr Sue Anne Toh and Dr Kyle Tan), dietitians and fitness instructors (Ruth Ho, Yap Mee Li, Sylvester Goh)
What is diabetes?
Diabetes is a condition characterised by high blood glucose (commonly referred to as sugar) levels. Glucose comes from the food we eat. It is also produced by our liver. Glucose is the main source of energy for the body’s cells and is transported through the bloodstream.
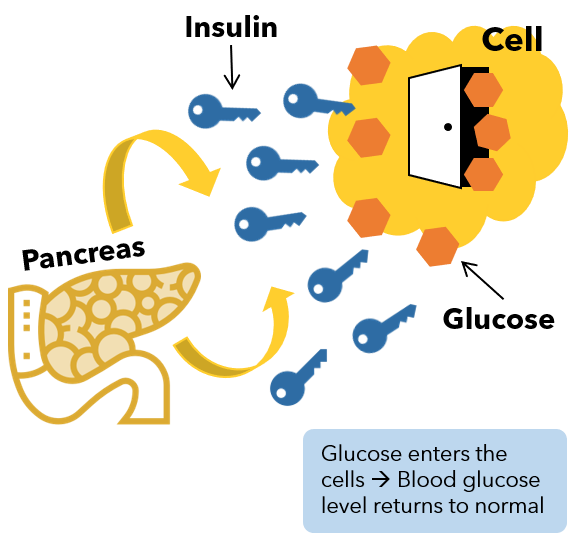
In order for our cells to use glucose, it needs to first enter our cells. Insulin is a hormone that is produced by our pancreas and it acts like a “key” to help glucose enter our cells.
Diabetes happens when our body either doesn’t make enough insulin (i.e. defect in insulin secretion), and/or it doesn’t use insulin well (i.e. insulin resistance). Without insulin, the cell remains locked, and glucose can’t get inside. The glucose remains in our blood and causes the high blood glucose (also known as high blood sugar) that we see in diabetes!
Figure 1. Insulin acts as a “key” to help glucose enter our cells. When insulin doesn’t work effectively, glucose stays in our blood, leading to high blood sugar.
Types of diabetes
Type 1 diabetes occurs when the body is unable to produce insulin. It can occur at any age, although it typically presents more commonly in children and young adults. Different factors, including genetics and some viruses, may contribute to type 1 diabetes (1).
Type 2 diabetes occurs when the body does not produce enough insulin or when the insulin produced does not work properly. Type 2 diabetes is the most common form of diabetes in the world, accounting for over 90% of all diabetes cases (2).
Gestational diabetes occurs when hormones produced during pregnancy causes our cells to be more resistant to insulin. Gestational diabetes increases the risk of complications during pregnancy and increases the risk of developing type 2 diabetes for both mother and baby (3).
Pre-diabetes is a condition where your blood glucose (sugar) level is higher than normal, but it’s not high enough to be considered diabetes. It is a warning sign for type 2 diabetes. Research has shown that about 70% of people with pre-diabetes will develop type 2 diabetes over time (4). With lifestyle changes, it is possible to prevent pre-diabetes from developing into type 2 diabetes (5).
Causes & risk factors for diabetes
You are more likely to develop type 2 diabetes if you have any of these risk factors:
You are aged 40 and above (6).
Your parent or sibling has type 2 diabetes (6).
You are overweight (6).
You are inactive (6)
You have high blood pressure (7) (greater than 140/90mmHg).
You have high levels of triglycerides (8).
You have low levels of high-density lipoprotein (HDL) (also known as “good cholesterol”) (9).
You have had gestational diabetes previously (6).
You smoke (6).
You have prediabetes (4).
Type 1 diabetes is mostly caused by genetic factors, while type 2 diabetes is mostly caused by poor eating and lifestyle habits. When we continuously consume more glucose than our body uses, our body has to increase the amount of insulin in our blood so that we can store the excess glucose. Over time, our cells become resistant to the effects of insulin (we call this insulin-resistance), causing the glucose to remain in our blood. This is why diet and lifestyle is often said to be the root cause of type 2 diabetes, and why dietary and lifestyle advice is important for the management of type 2 diabetes!
Signs and symptoms of type 1 and type 2 diabetes
Symptoms of diabetes include:
Slow-healing wounds or frequent infections.
Being hungrier and thirstier than usual.
Having to urinate more frequently.
Blurred vision.
Fungal infection, itching of skin and genitals.
Losing weight in spite of eating more.
Numbness of hands and feet.
If you experience any of these symptoms, consider consulting a doctor.
More often than not, diabetes is asymptomatic - this is why regular health screening is important to pick diabetes.
How do I know if I have diabetes?
Diabetes is common in Singapore - 1 out of every 9 Singaporeans affected by it. Diabetes often does not present with any obvious symptoms or signs especially early on. Regular health screening is hence important to detect diabetes early. You should go for health screening annually if you have any of the risk factors listed above. Otherwise, stick to the recommended screening schedule.
Diabetes can be diagnosed in the following ways:
Fasting blood sugar test. Your blood sample is taken after an overnight fast (at least eight hours). A reading of less than 5.6 mmol/L (100 mg/dL) is normal. A level from 5.6 to 6.9 mmol/L (100 to 125 mg/dL) indicates prediabetes. If your fasting blood sugar is 7 mmol/L (126 mg/dL) or higher on two separate tests, you have diabetes.
Casual blood sugar test. This is the same as fasting blood sugar test, except that you do not need to fast overnight. A reading of more than 11.1 mmol/L (200 mg/dL) means you have diabetes.
Glycated hemoglobin (HbA1C) test. This blood test indicates your average blood sugar level for the past two to three months. Normal levels are below 5.7%, and a result between 5.7 and 6.4% is considered prediabetes. A HbA1c level of 6.5% or higher suggests you have diabetes. You may be advised to undergo an oral glucose tolerance test for confirmation.
Oral glucose tolerance test. For this test, you will need to fast overnight and then drink a sugary liquid at the doctor's office. Blood sugar levels are tested before the sugary drink and two hours after the drink. For the first reading, a reading of less than 5.6 mmol/L (100 mg/dL) is normal. A level from 5.6 to 6.9 mmol/L (100 to 125 mg/dL) indicates prediabetes. A reading of 7 mmol/L (126 mg/dL) or higher suggests you have diabetes. For the second reading (two hours after taking the sugary drink), a blood sugar level less than 7.8 mmol/L (140 mg/dL) is normal. A reading between 7.8 mmol/L and 11.0 mmol/L (140 and 199 mg/dL) indicates prediabetes. A reading of 11.1 mmol/L (200 mg/dL) or higher after two hours suggests diabetes.
How can diabetes harm you?
A high level of glucose in our blood causes damage to our cells and blood vessels. That is why many people with poorly controlled diabetes find themselves developing severe complications. Diabetes is a leading cause of kidney failure, blindness, lower limb amputation, heart attack and stroke (10). In Singapore, 1 in 2 people who had a heart attack had coexisting diabetes, and 2 in 3 new cases of kidney failure had diabetes (11).
Complications of diabetes include:
Heart and blood vessel (cardiovascular) disease. Damage to blood vessels increases the risk of heart disease, high blood pressure, narrowing of blood vessels (atherosclerosis), stroke and heart attack.
Nerve damage (neuropathy). Damage to the nerves can result in tingling, numbness, burning or pain that usually starts at the tips of the toes or fingers and gradually spreads upward. Eventually, you may lose all sense of feeling in the affected limbs. For men, damage to nerves and blood vessels may result in erectile dysfunction.
Kidney damage (nephropathy). Damage to the blood vessels that supply blood to the kidneys may lead to kidney damage. In severe cases, this can lead to kidney failure, which may require dialysis or a kidney transplant. Dialysis is a hugely expensive treatment and often causes a huge impact to a person’s financial stability as well as quality of life.
Eye damage (retinopathy). Damage to the blood vessels that supply blood to the eyes may lead to serious eye diseases, such as cataracts and glaucoma. Diabetes could potentially lead to blindness if the blood vessels of the retina get damaged.
Amputations. High blood sugar level causes wounds to heal slower than usual when the blood vessels that supply blood to the wounded area get damaged. Due to the slow healing, wounds have an increased risk of getting infected, and these infections tend to get worse over time. In severe cases the infection may become so bad that the affected area needs to be amputated to prevent further spread of the infection. This happens most frequently to the extremities of our body such as the toes and feet. In severe situations the whole leg may become infected and needs to be amputated.
Two large-scale studies – the UK Prospective Diabetes Study (UKPDS) and the Diabetes Control and Complications Trial (DCCT) – demonstrated that improving HbA1c by 1% for people with type 1 diabetes or type 2 diabetes cuts the risk of microvascular complications by 25%.
Microvascular complications include:
Retinopathy
Neuropathy
Diabetic nephropathy
Research has also shown that people with type 2 diabetes who reduce their HbA1c level by 1% are:
19% less likely to suffer cataracts
16% less likely to suffer heart failure
43% less likely to suffer amputation or death due to peripheral vascular disease.
What is life like with diabetes?
Getting diagnosed with diabetes often comes as a shock and can be overwhelming. After getting over the initial shock, you and your loved ones may have many questions in your mind. What does diabetes mean for me and my loved ones? Is it a reversible condition? Will I be on medication for the rest of my life? Will I still be able to enjoy the foods I like?
It is important to get good support during this time to reduce the stress and to understand how best to improve your health. A healthcare provider and team with the right skillset can make a big difference (read more on that here).
You may also wish to learn and read more about diabetes on your own. There are good resource hubs such as the Health Promotion Board, NHS Diabetes and US CDC websites which are regularly updated and full of user friendly information. In this article, we share some of the basics of diabetes and you can find out more through our health library and filtering for the appropriate topic.
What can I do to manage and control my diabetes?
Diabetes is known as a lifestyle disease because our lifestyle is the biggest contributor to the development and severity of diabetes. In order to control your blood sugar, you may be advised to “eat healthier” or “exercise more”. In this section we hope to provide you with more concrete tips on how to make small changes to various aspects of your lifestyle so that you can improve your blood sugar control, as well as outline the medical therapy, monitoring and follow-ups that are important in diabetes management.
Diet
Contrary to popular belief, there's no magic diet that will reverse diabetes or improve sugar control. The best diet is always the diet that works for you and your unique circumstances. That said, here are some important principles to center your diet around:
Fewer calories
Fewer refined carbohydrates, especially those with added sugars
Fewer foods containing saturated fats
More vegetables and fruits
More foods with fibre
Adequate protein
A dietitian or nutritionist can help you put together a meal plan that fits your health goals, food preferences and lifestyle. He or she can also teach you how to monitor your carbohydrate intake and teach you dietary strategies to keep your blood sugar levels more stable.
Read more about how to eat well if you have diabetes here.
Exercise
When you exercise, your muscles use glucose for energy, lowering your blood sugar level. Regular exercise can also build muscles, helping your body better respond to insulin and also utilize more glucose. These factors combined will help you to better control your blood sugar levels. On top of that exercising can help you to lose weight, look better and feel healthier. Talk about a win-win!
Aim for at least 150 minutes of moderate intensity physical activity (e.g. brisk walking) per week, and at least 2 sessions of strength/resistance training a week.
Weight Loss
If you are overweight, losing just 5 - 7% of your weight can make a difference to the control of your diabetes. If you are of Asian ethnicity, your body mass index (BMI) should be below 23 as a guide. If you are of other ethnicities, you can aim for a BMI of 25 and below.
Losing weight can be difficult, but it brings many benefits. You look better, feel better and most importantly, get healthier. Losing weight can improve diabetes control and reduce the risk of developing diabetes related complications.
To learn about our guided weight loss program, click here.
Smoking
Smoking impairs insulin sensitivity and secretion. Therefore it is very helpful to reduce or stop smoking for people with diabetes. This is a challenging task and it would be ideal to sign up for a guided program that can teach you different strategies for quitting. Singapore’s Health Promotion Board (HPB) has a great 28 days program that you can sign up for here.
Alcohol
Alcohol is a high calorie drink that can cause your blood sugar to spike after consumption. Long term consumption of alcohol may also affect your body’s ability to release glucose from cells when needed, which can lead to low blood sugar - a condition that can cause dizziness and even coma.If you need to consume alcohol, you should have no more than 1 drink per day if you are female, and no more than 2 drinks per day if you are male. A standard drink is one can (330ml) of beer, one glass (100ml) of wine, or one nip (30ml) of spirits.
Medication
Some people who have type 2 diabetes can achieve their target blood sugar levels through diet, exercise and weight loss alone. However, many also need diabetes medications or insulin therapy.
Many people with diabetes wonder what is the best diabetes medication. While there is no “best” medication, some medicines may work better for you. The decision on which medications are best suited for you depends on many factors, including your lifestyle factors, underlying root causes of diabetes, your blood sugar level and any other health problems you have. Your doctor will suggest the appropriate medication based on these factors, and might even combine drugs from different classes to help you control your blood sugar in several different ways.
Monitoring blood sugar
HbA1c allows clinicians to get an overall picture of what your average blood sugar levels have been over a three month period. This is important as it gives an indication of how the diabetes control has been and whether modification to the treatment is needed. The higher the HbA1c, the greater the risk of developing diabetes-related complications.
HbA1c levels need to be checked between two and four times a year. Discuss your target HbA1c goal with your doctor, as it may vary depending on your age and other factors. For most people, the American Diabetes Association recommends an HbA1c level below 7%. An elevated HbA1c level may signal the need for a change in your medication, diet or activity level.
For most persons with diabetes, it is also important to monitor your glucose levels at home. Monitoring your glucose levels in between doctor’s visits will allow you to get a sense of how well your glucose control is, and allows adjustment of food choices and medication dosage in a timely fashion. Self monitoring is done by pricking your finger with a small needle called a lancet, drawing a drop of blood from the finger and applying it to a test strip placed in a glucometer. How frequently you need to check your blood glucose depends on your condition. Discuss this with your doctor. Read our article on glucose monitoring for a more complete guide to self monitoring and tips on what to do when facing common high glucose level scenarios.
Alternatively, new options for self monitoring include use of a Flash Glucose Monitor (FGM). The FGM is applied on your arm, and is able to continuously measure your glucose level while eliminating the need for finger pricks. This provides you with a more complete picture of how your glucose levels are changing with the food you eat, your activity levels and medication, opening up opportunities for more personalized treatment plans.
Regular check ups
It is important to follow up with your doctor at least every 3 to 6 months so that they can ensure that your blood sugar is controlled adequately and update your treatment plan if needed.
You should also get your kidney function, feet and eyes checked yearly to detect early signs of diabetes-related complications.
Learn about diabetes management
There’s a lot to share when it comes to managing diabetes. Through our interactions with thousands of individuals with diabetes, we constantly come up with practical tips for improving blood sugar control. Check out our blog and subscribe to our newsletter to keep yourself updated!

Success story
Watch how our patient Mr Png managed to get his blood sugar levels from 12.9% to 5.6% through a combination of medical therapy, diet and lifestyle changes.
NOVI Magnum
If you are looking for a treatment plan that combines medical, diet and fitness advice, check out NOVI Magnum - our holistic diabetes management program. Our specialist doctors and dietitians will work together with you as a team to help you craft a personalised treatment plan that works for you.
References
Atkinson, M.A., Eisenbarth, G.S. and Michels, A.W. (2014). Type 1 diabetes. The Lancet, [online] 383(9911), pp.69–82. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4380133/.
National Collaborating Centre for Chronic Conditions (UK) (2008). Type 2 Diabetes: National Clinical Guideline for Management in Primary and Secondary Care (Update). [online] Available at: https://www.ncbi.nlm.nih.gov/pubmed/21678628 [Accessed 29 Mar. 2019].
American Diabetes Association. Gestational diabetes mellitus. Diabetes Care 2003;26(Suppl. 1):s103–s105. Available at: https://care.diabetesjournals.org/content/26/suppl_1/s103
Ligthart, S., van Herpt, T.T.W., Leening, M.J.G., Kavousi, M., Hofman, A., Stricker, B.H.C., van Hoek, M., Sijbrands, E.J.G., Franco, O.H. and Dehghan, A. (2016). Lifetime risk of developing impaired glucose metabolism and eventual progression from prediabetes to type 2 diabetes: a prospective cohort study. The Lancet Diabetes & Endocrinology, [online] 4(1), pp.44–51. Available at: https://www.thelancet.com/journals/landia/article/PIIS2213-8587(15)00362-9/fulltext [Accessed 1 Dec. 2019].
https://www.ncbi.nlm.nih.gov/pubmed/11832527.
Galtier, F. (2010). Definition, epidemiology, risk factors. Diabetes & Metabolism, 36(6), 628–651. Available at: https://europepmc.org/article/med/21163426 [Accessed 12 May 2020].
Kim, M.-J., Lim, N.-K., Choi, S.-J. and Park, H.-Y. (2015). Hypertension is an independent risk factor for type 2 diabetes: the Korean genome and epidemiology study. Hypertension Research, [online] 38(11), pp.783–789. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4644940/.
Tirosh, A., Shai, I., Bitzur, R., Kochba, I., Tekes-Manova, D., Israeli, E., Shochat, T. and Rudich, A. (2008). Changes in Triglyceride Levels Over Time and Risk of Type 2 Diabetes in Young Men. Diabetes Care, [online] 31(10), pp.2032–2037. Available at: https://care.diabetesjournals.org/content/31/10/2032 [Accessed 17 Nov. 2019].
Perry, I.J., Wannamethee, S.G., Walker, M.K., Thomson, A.G., Whincup, P.H. and Shaper, A.G. (1995). Prospective study of risk factors for development of non-insulin dependent diabetes in middle aged British men. BMJ : British Medical Journal, [online] 310(6979), pp.560–564. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2548938/ [Accessed 12 May 2020].
https://www.who.int/news-room/fact-sheets/detail/diabetes.
National Registry of Diseases Office, 2014, Singapore.
https://www.healthxchange.sg/diabetes/essential-guide-diabetes/what-is-prediabetes-what-do-when-diagnosed
https://www.sgh.com.sg/patient-care/specialties-services/Pathology/Pages/GLUCOSE-TOLERANCE-TEST-PLASMA.aspx
American Diabetes Association